Inhaled form of COVID-19 vaccine developed in Hamilton more effective than injection: McMaster University study
Published February 9, 2022 at 11:12 am
McMaster University scientists in Hamilton have confirmed that their inhaled form of COVID vaccine can provide broad, long-lasting protection against the original strain of SARS-CoV-2 and variants of concern.
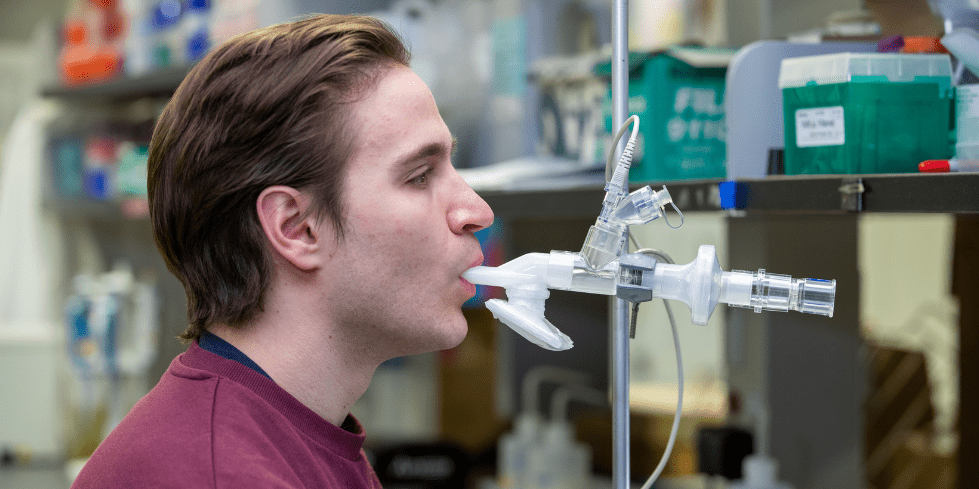
The vaccine is inhaled directly into the respiratory tract, and researchers say they revealed immune mechanisms and significant benefits compared to the traditional injecting of the vaccine. This is because inhaled vaccines target the lungs and upper airways where respiratory viruses first enter the body. Researchers say it’s a far more effective way of inducing a protective immune response.
Clinical trials are now underway to evaluate inhaled aerosol vaccines in healthy adults who had already received two doses of a COVID mRNA vaccine.
The tested COVID vaccine strategy was built upon a tuberculosis vaccine research program established by Zhou Xing, a co-lead author of the new study and a professor at the McMaster Immunology Research Centre and Department of Medicine.
“What we’ve discovered from many years’ research is that the vaccine delivered into the lung induces all-around protective respiratory mucosal immunity, a property that the injected vaccine is lacking,” Xing says. “We have revealed in our report that besides neutralizing antibodies and T cell immunity, the vaccine delivered into the lungs stimulates a unique form of immunity known as trained innate immunity, which is able to provide very broad protection against many lung pathogens besides SARS-CoV-2.”
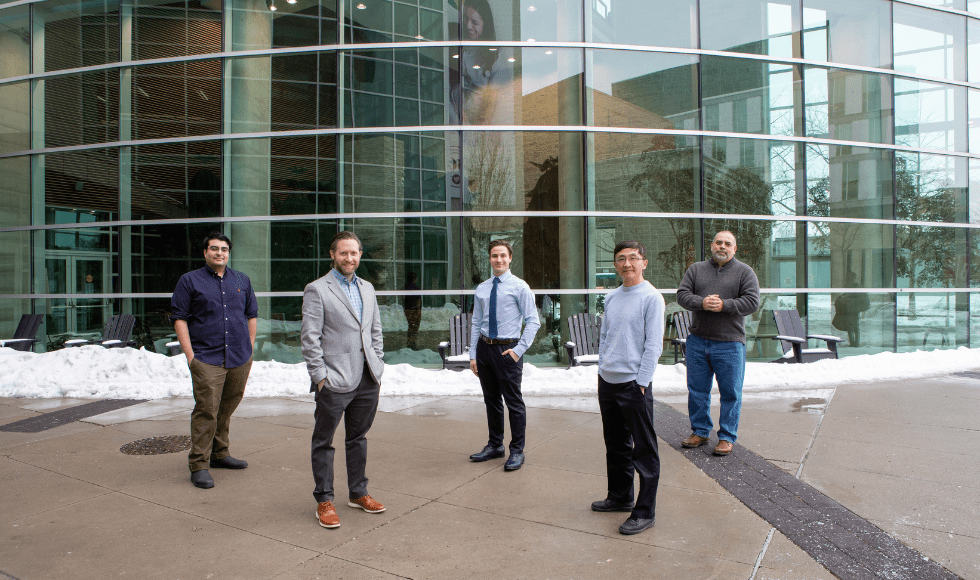
From left to right: Researcher Sam Afkhami, study co-lead Matthew Miller, researcher Michael D’Agostino, and study co-leads Zhou Xing and Brian Lichty outside the Michael DeGroote Centre for Learning and Discovery at McMaster University. (Photo by Georgia Kirkos/McMaster University)
The study’s co-lead author Matthew Miller, an associate professor at McMaster’s Michael G. DeGroote Institute for Infectious Disease Research, added that the research team wanted to design a vaccine that would work well against any variant.
“We can remain ahead of the virus with our vaccine strategy,” says Miller. “Current vaccines are limited because they will need to be updated and will always be chasing the virus.”
All COVID vaccines currently approved in Canada target only the spike protein, which has shown the ability to mutate.
The new McMaster vaccine is effective against highly transmissible variants because they are designed to target three parts of the virus, including two that are highly conserved among coronaviruses and do not mutate as quickly as the spike.
“This vaccine might also provide pre-emptive protection against a future pandemic, and that’s really important because as we’ve seen during this pandemic – and as we saw in 2009 with the swine flu – even when we are able to rapidly make a vaccine for a pandemic virus, it’s already way too late. Millions of people died, even though we were able to make a vaccine in record time,” says Miller.
In addition to being needle and pain-free, an inhaled vaccine is efficient at targeting the lungs and upper airways that it can achieve maximum protection with a small fraction of the dose of current vaccines – possibly as little as 1 per cent – meaning a single batch of vaccine could go 100 times farther, the researchers say.
The research was published on the Cell and can be read online.
The McMaster COVID vaccine represents one of only a handful developed in Canada. It’s part of Canada’s Global Nexus for Pandemics and Biological Threats, which is based at McMaster.
The vaccines were manufactured at the Robert E. Fitzhenry Vector Laboratory in Hamilton.
The research is funded by a CIHR COVID-19 Rapid Response grant.
insauga's Editorial Standards and Policies advertising